Information for Patients
You’re not alone, and you are not dismissed—even when doctors can’t give you a clear diagnosis. Tune into your body’s signals and work with experts to uncover what they mean. Discover the language of your body by exploring our guide.
New or suddenly severe symptoms should be assessed promptly—e.g., crushing chest pain, one-sided weakness or speech trouble, fainting, severe breathlessness, high fever, blood in vomit/stool/urine, persistent vomiting, or unexplained weight loss. Safety first.
-
It’s a quite common and confusing situation. Medical investigations are excellent at finding structural problems—like infections, inflammation, or tissue damage. But many symptoms come from functional changes in how your body is working (for example, a stress-response and nervous system stuck on “high alert”). Those changes are real, yet they often don’t show up on scans or standard blood tests.
Important nuance about “negative” results
A normal test today doesn’t always rule out an organic illness. Some conditions are missed in early phases, and many diseases are dynamic—results can “turn positive” over days or weeks as changes evolve.
Any acute (new, sudden, or rapidly worsening) symptom should be assessed—and sometimes re-assessed—promptly. Safety first.
When to consider a psychosomatic (mind–body) explanation
When symptoms persist for a long time—either continuously or on-and-off—typically longer than 2–3 months (and often years), and repeated investigations remain negative.
In this scenario, a mind–body pattern becomes more likely and, importantly, treatable.
Key reassurance: a normal work-up does not invalidate your suffering. It often points to a functional, mind–body cause. It is common, understandable, and manageable with the right support.
-
Psychosomatic syndromes are conditions where stress, emotions, and learned body-responses change how your body works—without causing structural damage. They can produce very real symptoms like pain, fatigue, gut upset, palpitations, dizziness, breathlessness, or brain fog.
Not “all in your head”
These conditions involve physiological changes: the stress system, autonomic nervous system, pain circuits, hormones, muscle tension, and gut motility can all shift into an over-protective “high alert” mode. That’s why you feel symptoms even though scans and blood tests are normal. Think of it as a sensitive alarm system—not a broken organ.Also safe—and reversible
While distressing, psychosomatic syndromes are generally safe: they don’t mean your body is being damaged. With the right support—education, stress regulation, pacing, sleep, movement, and therapies that calm and retrain the nervous system—symptoms can improve and often resolve. (If new or suddenly worsening symptoms appear, a clinician should still check them.) -
Many everyday health complaints can be functional—driven by a sensitised stress/nervous system rather than structural damage. Common examples include:
Pain: tension-type headaches or migraines; neck, back or shoulder pain; widespread muscle/joint aches; jaw/TMJ pain; chest pain with normal heart tests.
Gut (IBS-type): abdominal pain or cramping, bloating, wind, diarrhoea/constipation, nausea, reflux—despite normal scopes/bloods.
Heart–lung sensations: palpitations, pounding heart, “skipped beats”; breathlessness, air hunger, frequent sighing, tight chest; hyperventilation.
Dizziness & balance: light-headedness, rocking/swaying, motion sensitivity, “brain fog.”
Neurological-type symptoms: tingling/numbness, limb heaviness or weakness, tremor or spasms, functional neurological symptoms (e.g., non-epileptic attacks, gait changes) after normal scans.
Sleep & energy: persistent fatigue, unrefreshing sleep, insomnia.
Pelvic & bladder: pelvic pain, urinary urgency/frequency, sexual dysfunction with normal tests.
Skin & temperature: itching without a rash, flushing, sweats or chills, temperature swings.
Ear/throat/eye: tinnitus, globus (lump-in-throat sensation), blurred focus, dry eyes/mouth.
-
You don’t have to feel stressed to have a functional condition. Somatisation can appear at any time in life, sometimes long after a difficult event or psychological trauma. The nervous system may have learned an “over-protective” pattern back then, and it can be re-triggered by illness, life changes, or even without a clear spark.
Why stress isn’t always obvious:
Hidden or habitual: Long-running pressure can feel “normal,” so you don’t notice it.
Delayed effects: Past losses, shocks or trauma can prime the body’s alarm system.
Suppressed or unclear emotions: Many of us push feelings down or struggle to name them; the body then speaks up with physical signals.
Focus on the physical: It’s natural to scan the body, not our emotional load.
-
These conditions trigger physiological changes: the stress response, autonomic nervous system, pain pathways, hormone levels, muscle tension, and gut motility can all enter a heightened, over-protective "high alert" state. This explains why symptoms persist even when scans and blood tests show no abnormalities. Imagine it as an overly sensitive alarm system, not a malfunctioning organ. Your symptoms, pain, and suffering are genuine. The key difference is their origin. By identifying the root cause, we can often resolve the problem.
-
For most people with psychosomatic (mind–body) symptoms, you are safe. These symptoms are driven by changes in how your stress and nervous systems are functioning, not by ongoing tissue damage. They can feel intense and scary, but they’re usually uncomfortable rather than dangerous.
That said, safety comes first:
A normal test today doesn’t always exclude an organic illness forever. Some conditions are missed early and results can “turn positive” over days or weeks as things evolve.
New, sudden, or rapidly worsening symptoms should be assessed—and sometimes re-assessed—promptly.
Seek urgent care (call emergency services) if you have:
Crushing/central chest pain, severe breathlessness, fainting, or a new fast/irregular heartbeat
One-sided weakness, facial droop, or speech trouble
Vomiting blood, black/bloody stools, severe persistent abdominal pain
High fever with a rash, new confusion, or the “worst headache” of your life
Unexplained, significant weight loss
When reassurance fits: if symptoms have persisted over 2–3 months (often on-and-off for longer) and repeated investigations remain normal, a mind–body explanation becomes more likely—and generally safe and treatable. Focus can shift to calming and retraining the system (education, stress regulation, sleep, pacing, gentle movement, and appropriate therapies) while staying alert to any genuinely new red flags.
-
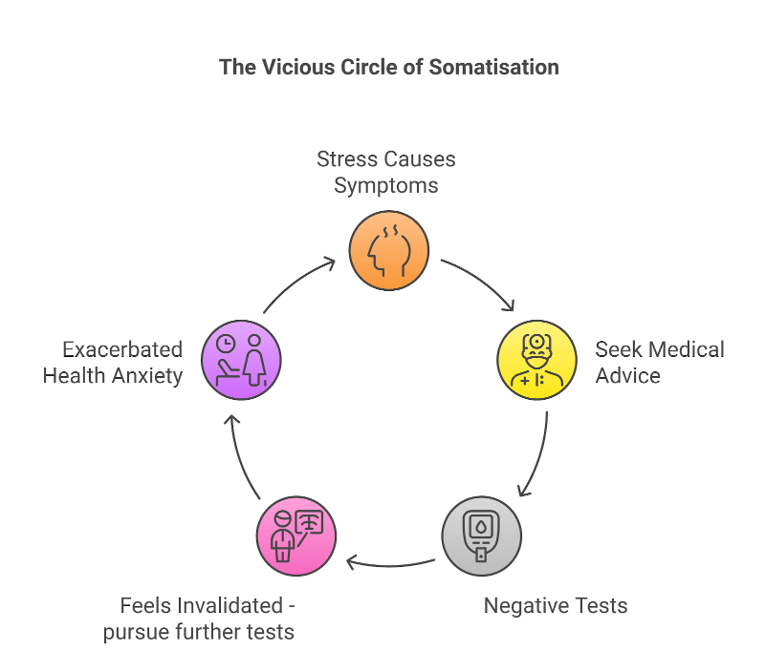
When symptoms are real but functional (mind–body) and this isn’t recognised, people can get trapped in a self-reinforcing loop (see the picture):
Stress → symptoms. The body’s alarm system goes on “high alert,” producing pain, palpitations, gut upset, dizziness, etc.
Seek medical advice.
Negative tests. Scans and bloods look normal because function—not structure—is the problem.
Feels invalidated → more tests. “No answer” can feel like “no one believes me,” so the search intensifies.
Health anxiety grows. Worry amplifies sensations, sleep worsens, activity drops.
More stress… more symptoms. The cycle restarts.
Why this matters
More investigations, cost and side-effects (including incidental findings and unnecessary procedures)
Greater fear and avoidance → deconditioning, social withdrawal, lower quality of life
Delayed access to treatments that actually help
-
It’s hard to diagnose. No simple test can prove a psychosomatic problem, so doctors use a mix of physical and mental evaluations. Also, they first check for the most serious organic illnesses.
There are a few other factors which makes doctors reluctant to make this diagnosis early:
Biomedical-first training: Doctors are taught to rule out organic disease first. Guidelines, tests and referrals are set up around this model.
Stigma & wording fears: Many clinicians worry that saying “psychosomatic” will be heard as “it’s all in your head,” risking mistrust—even though that’s not what it means.
Medico-legal caution: “What if I missed something?” leads to repeat tests or referrals, especially early on when illnesses can still declare themselves.
Time & pathway gaps: Short appointments and limited training/services for functional disorders make the conversation and follow-up harder.
Diagnostic timeline: A mind–body diagnosis is usually made after symptoms persist (often >2–3 months) and tests stay normal; acute or new symptoms must still be checked and sometimes re-checked.
Bottom line: your symptoms are real and usually safe. Inviting your clinician to discuss a both/and approach—ruling out danger and addressing mind–body factors—often opens the door to effective treatment.
-
Name it: a functional, mind–body pattern—real, common, and usually safe
Plan care: one lead clinician, safety-netting for any new/rapidly worsening symptoms
Retrain the system: education, stress regulation, pacing, sleep, gentle graded activity, physiotherapy, and therapies like CBT or similar
Address drivers: life stressors, grief/trauma, health anxiety, perfectionism
Reduce unnecessary tests once danger is reasonably excluded, and focus on recovery skills instead
-
The initial step on the path to healing is grasping the mind-body connection. Having more questions is actually a positive sign—it reflects your curiosity and dedication to challenging stigma while actively participating in the recovery process of medically unexplained symptoms. For comprehensive answers, explore my book Undiagnosed (available on Amazon) or enroll in our course.
Break the cycle - Self Care Advice
“Every day I walk myself into a state of well-being and walk away from every illness”
Lifestyle changes are practical tools to calm an over-alert nervous system and support your medical care.
They give you safe, evidence-informed ways to reduce stress reactivity and break the cycle of somatisation.
We’ll focus on small, achievable steps across sleep, stress management, physical activity, nourishing food, and supportive relationships.
Start with one or two actions you can repeat daily, then build gradually.
Use this section alongside your clinician’s advice, and be kind to yourself—progress is measured over weeks, not days.
Listen to the 5-minute podcast that sums up the 5+1 lifestyle changes and tells you where to begin.
Professional Help
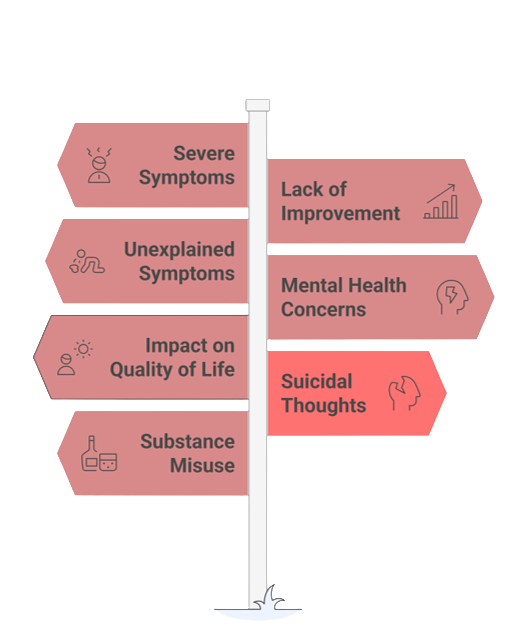
Red Flags - when you must seek for professional help
If recurrent, test-negative symptoms persist beyond 4–6 weeks, intensify, or begin to limit daily life (missing work/school, avoiding activity or travel), it’s time to seek help.
Book a medical review if you’re preoccupied with health (constant body-checking, frequent reassurance-seeking, repeated online searches or clinic/A&E visits) or using alcohol/sedatives to cope.
Arrange psychological support when symptoms follow stress or trauma, when emotions feel “stuck” or hard to name, or when low mood, anxiety, poor sleep, irritability, or hopelessness accompany the physical complaints. Any thoughts of self-harm require urgent help.
And always treat classic medical red flags (e.g., chest pain, severe breathlessness, one-sided weakness, black or blood-stained stools, “worst-ever” headache) as emergencies.
Ask your GP to rule out disease and coordinate evidence-based mind–body care (e.g., CBT/ACT, trauma-focused therapy, mindfulness/relaxation, graded activity)